Foot pain
Highlights
Overview
- The foot is a complex structure of 26 bones and 33 joints, layered with an intertwining web of more than 120 muscles, ligaments, and nerves.
- The foot serves the following functions:
- Supports weight
- Acts as a shock absorber
- Serves as a lever to propel the leg forward
- Helps maintain balance by adjusting the body to uneven surfaces
- Nearly all cases of foot pain can be attributed to one of the following:
- Ill-fitting shoes
- High-impact exercise
- Certain medical conditions.
Risk Factors
- Elderly people are at very high risk for foot problems.
- Women are at higher risk than men for severe foot pain, probably because of high-heeled shoes.
- Some people have turned to cosmetic surgery as a drastic way to fit into high-heeled shoes. The American Orthopaedic Foot and Ankle Society strongly advises against cosmetic foot surgery and urges consumers to carefully consider the relative risks and benefits of undergoing unnecessary surgical procedures.
- Medical Conditions Causing Foot Pain
- Arthritis
- Diabetes
- Obesity
- Pregnancy
- Medications
Treatment
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen (Advil), may help ease pain and reduce inflammation.
- The acronym RICE stands for rest, ice, compression, and elevation -- the four basic elements of initial treatment for an injured foot.
- For severe conditions, such as fallen arches or structural problems that cause imbalance, podiatrists or physicians may need to prescribe custom orthotics, which are insoles produced to fit the patient's foot.
Prevention
- Don't ignore foot pain -- it's not normal.
- It is critical that people with diabetes see a podiatric physician at least once a year for a checkup.
Introduction
Foot pain is very common. About 75% of people in the United States have foot pain at some time in their lives. Most foot pain is caused by shoes that do not fit properly or that force the feet into unnatural shapes (such as pointed-toe, high-heeled shoes).
The foot is a complex structure of 26 bones and 33 joints, layered with an intertwining web of more than 120 muscles, ligaments, and nerves. It serves the following functions:
- Supports weight
- Acts as a shock absorber
- Serves as a lever to propel the leg forward
- Helps maintain balance by adjusting the body to uneven surfaces
Because the feet are very small compared with the rest of the body, the impact of each step exerts tremendous force upon them. This force is about 50% greater than the person's body weight. During a typical day, people spend about 4 hours on their feet and take 8,000 - 10,000 steps. This means that the feet support a combined force equivalent to several hundred tons every day.
Foot Problems and Their Locations
Foot pain generally starts in one of three places: the toes, the forefoot, or the hindfoot.
The Toes. Toe problems most often occur because of the pressure imposed by ill-fitting shoes.
The Forefoot. The forefoot is the front of the foot. Pain originating here usually involves one of the following bone groups:
- The metatarsal bones (five long bones that extend from the front of the arch to the bones in the toe)
- The sesamoid bones (two small bones embedded at the top of the first metatarsal bone, which connects to the big toe)
The Hindfoot. The hindfoot is the back of the foot. Pain originating here can extend from the heel, across the sole (known as the plantar surface), to the ball of the foot (the metatarsophalangeal joint).
Summary of Foot Problems
Condition | Location | Symptoms | Recommended Footwear | |
Toe Pain | ||||
Corns and calluses | Around toes, usually little toe, bottom of feet or areas exposed to friction. | Hard, dead, yellowish skin. | Wide (box-toed) shoes; soft cushions under heel or ball of foot, or customized or gel insoles for calluses. Doughnut-shaped pads for corns. | |
Ingrown toenails | Toenails. | Nail curling into skin causes pain, swelling, and, in extreme cases, infection. | Sandals, open-toed shoes. | |
Bunions and bunionettes (tailor's bunion) | Big toe (bunions) or little toe (bunionettes). | The following can occur alone or in combination: Metatarsus primus varus. The first (big toe) metatarsal bone shifts away from the second, and the big toe points inward. Medial exostosis. This is a bony bump at the base of the big toe, which protrudes outward. Area next to bony bump is red, tender, and occasionally filled with fluid. Toe joint may be inflamed. Hallux valgus. This is a deformity in which the bone and joint of the big toe shift and grow inward, so that the second toe crosses over the big toe. | Soft, wide-toed shoes or sandals. Bunion shields or splints. Thick doughnut-shaped moleskin pads, custom-made orthotics or foot slings, if necessary. Avoid shoes with stitching along the side of the "bump." | |
Morton's neuroma (also called interdigital neuroma) | Inflammation of the nerve, usually between the third and fourth toes and bottom of the foot near these toes. | Cramping and burning pain, or electric-shock sensation. The condition may produce a thick protective sheath around the nerve that feels like a ball. This may be detected by pressing top to bottom on the top of the foot using one hand and moving the other hand from side to side. Morton's neuroma is aggravated by prolonged standing and relieved by removal of the shoes and forefoot massage. | Wide (box-toed) shoes. Orthotic or insole with pad that reduces stress on the painful area. | |
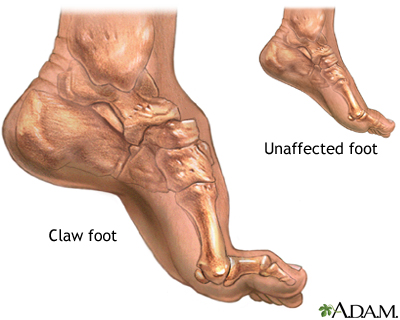
Hammertoe or claw toe | Usually second toe, but may develop in any or all of the three middle toes. | Toes form hammer or claw shape. In hammertoe, the first knuckle of the toe is mainly affected. In claw toe the entire toe is deformed. No pain at first, but pain increases as tendon becomes tighter and toes stiffen. | Wide (box-toed) shoes. Toe pads or specially designed shields, splints, caps, or slings. (Splints or slings are not for people with diabetes.) | |
Front-of-the-Foot Pain | ||||
Metatarsalgia | Ball of the foot. | Acute, recurrent, or chronic pain without a known cause. | Wide (box-toed) shoes. Orthotic with pad that reduces metatarsal pressure. Gel cushions. Metatarsal bandage. | |
Stress fracture | Most often in the area beneath the second or third toe. | Sudden pain (which persists) when injury occurs. | Low-heeled shoes with stiff soles. | |
Sesamoiditis | Ball of foot beneath big toe. | Pain and swelling. | Low-heeled shoe with stiff sole and soft padding inside. | |
Heel and Back-of-the-Foot Pain | ||||
Plantar fasciitis or heel spurs | Back of the arch right in front of heel. | At onset, some people report a tearing or popping sound. Pain is most severe with first steps after getting out of bed. Pain decreases after stretching, returns after inactivity. | Over-the-counter foot insole (cut quarter-size hole surrounding painful area). Possible night splints. Orthotics if necessary. | |
Bursitis of the heel | Center of the heel. | Pain, with warmth and swelling. Increases during the day. | Heel cup. | |
Haglund's deformity ("pump bump") | Fleshy area on the back of the heel. | Tender swelling aggravated by shoes with stiff backs. | Soft shoes. Heel pads. Possible orthotic to support heel. | |
Achilles tendinitis | Achilles tendon: area along the back between calf muscles and heel. | Pain worsens during physical activities (particularly running), after which the tendon usually swells and stiffens. If it ruptures, popping sound may occur followed by acute pain similar to a blow at the back of the leg. | Insoles, tendon strap, heel cups. | |
Arch and Bottom-of-the Foot Pain | ||||
Tarsal tunnel syndrome | Anywhere along the bottom of the foot. | Numbness, tingling, or burning sensations, pain, most commonly felt at night. | Specially designed orthotics to relieve pressure. | |
"Flat feet" or posterior tibial tendon dysfunction (PTTD) | The arch. | No arch. Often no pain or discomfort. Three stages in PTTD: Pain and weakness in the tendon. The arch flattens but is still flexible. The foot becomes rigid and possibly painful at the ankle. Sometimes people report fatigue, pain, or stiffness in the feet, legs, and lower back. | For children, possible custom-made insoles. | |
High arches ("hollow feet") | The arch. | High arches. Lower back pain, possible tendency to lower limb injuries. | ||
Causes
Nearly all causes of foot pain can be grouped under one of the following:
- Ill-fitting shoes. Poorly fitting shoes are a frequent cause of foot pain. High-heeled shoes concentrate pressure on the toes and can aggravate, if not cause, problems with the toes.
- Certain medical conditions. Any medical condition that causes a disturbance in the way a person walks can contribute to foot pain. This may include diseases or conditions that lead to pain or numbness in the feet (such as diabetes), leg and foot deformities, spinal problems, and neurological disorders such as Parkinson's disease or cerebral palsy.
- High-impact exercise. High-impact exercising, such as jogging or strenuous aerobics, can injure the feet and other parts of the leg. Common injuries include corns, calluses, blisters, muscle cramps, acute knee and ankle injuries, plantar fasciitis, and metatarsalgia.
Medical Conditions Causing Foot Pain
Arthritic Conditions. Arthritic conditions, particularly osteoarthritis and gout, can cause foot pain. Although rheumatoid arthritis almost always develops in the hand, the ball of the foot can also be affected.
Diabetes. Diabetes is an important cause of serious foot disorders. [For more information, see In-Depth Report #9: Diabetes - type 1 and In-Depth Report #60: Diabetes - type 2.]
Obesity. Obesity can cause foot and ankle pain.
Pregnancy. Pregnancy can cause fluid buildup and swollen feet. The increased weight and imbalance of pregnancy contributes to foot stress.
Medications. Some medications, such as calcitonin and drugs used for high blood pressure, can cause foot swelling.
Risk Factors
A risk factor is anything that increases your chances of getting a disease or condition. The following are factors that increase your risk for foot pain:
Age
Elderly people are at very high risk for foot problems. As you age, your feet widen and flatten, and the fat padding on the sole of the foot wears down. The skin on the feet also becomes dryer. Foot pain in older adults may be the first sign of age-related conditions, such as arthritis, diabetes, and circulatory disease. Foot problems can also impair balance and function in this age group.
Cosmetic Foot Surgery
Taking fashion to extreme limits, some people have turned to cosmetic surgery as a drastic way to fit into high-heeled shoes. Procedures include surgical shortening of the toes, narrowing of feet, or injecting silicone into the pads of the feet. Such methods may increase your risk for future foot pain. The American Orthopaedic Foot and Ankle Society (AOFAS) and other foot-related medical associations have expressed concern over this trend. The AOFAS strongly advises against cosmetic foot surgery and urges consumers to carefully consider the relative risks and benefits of undergoing unnecessary surgical procedures.
Gender
Women are at higher risk than men for severe foot pain, probably because of high-heeled shoes. Severe foot pain appears to be a major cause of general disability in older women.
Occupational Risk Factors
An estimated 120,000 work-related foot injuries occur every year, about a third of them involving the toes. Many foot problems -- including arthritis of the foot and ankle, toe deformities, pinched nerves between the toes, plantar fasciitis, adult-acquired flat foot, and tarsal tunnel syndrome -- have been attributed to repetitive use at work (for example, walking long distances or standing for many hours). No studies, however, have scientifically distinguished between injuries due to work versus those due to regular use. This is an important issue because of its potential impact on disability claims.
Pregnancy
Pregnant women have an increased risk of foot problems due to weight gain, swelling in their feet and ankles, and the release of certain hormones that cause ligaments to relax. These hormones help when bearing the child, but they can weaken the feet.
Sports and Dancing
People who engage in regular high-impact aerobic exercise are at risk for plantar fasciitis, heel spurs, sesamoiditis, Achilles tendinitis, and stress fractures. Women are at higher risk for stress fractures than men.
Weight gain
Gaining weight puts added stress on the feet and can lead to foot or ankle injuries. The added pressure on the soft tissues and joints of the foot in overweight people increases the likelihood of developing tendinitis and plantar fasciitis.
Corns and Calluses
A corn is a protective layer of dead skin cells that forms due to repeated friction. It is cone-shaped and has a knobby core that points inward. This core can put pressure on a nerve and cause sharp pain. Corns can develop on the top of, or between, toes. If a corn develops between the toes, it may be kept pliable by the moisture from perspiration and is therefore called a soft corn.
Corns develop as a result of friction from the toes rubbing together or against the shoe. They often occur from the following:
- Shoes, socks, or stockings that fit too tightly around the toes
- Pressure on the toes from high-heeled shoes
- Shoes that are too loose, due to the friction of the foot sliding within the shoe
- Deformed and crooked toes
Calluses are composed of the same material as corns. Calluses, however, develop on the ball or heel of the foot. The skin on the sole of the foot is ordinarily about 40 times thicker than the skin anywhere else on the body, but a callus can even be twice as thick. A protective callus layer naturally develops to guard against excessive pressure and chafing as people get older and the padding of fat on the bottom of the foot thins out. If calluses get too big or too hard, they may pull and tear the underlying skin.
Risk factors for calluses include the following:
- Poorly fitting shoes
- Walking regularly on hard surfaces
- Flat feet
Of note, in people with diabetes, the presence of calluses is a strong predictor of ulceration, particularly in those who have a history of foot ulcers.
Preventing Corns and Calluses and Relieving Discomfort. To prevent corns and calluses and relieve discomfort if they develop:
- Do not wear shoes that are too tight or too loose. Wear well-padded shoes with open toes or a deep toe box (the part of the shoe that surrounds the toes). If necessary, have a cobbler stretch the shoes in the area where the corn or callus is located.
- Wear thick socks to absorb pressure, but do not wear tight socks or stockings.
- Apply petroleum jelly or lanolin hand cream to corns or calluses to soften them.
- Use doughnut-shaped pads that fit over a corn and decrease pressure and friction. They are available at most drug stores.
- Place cotton, lamb's wool, or mole skin between the toes to cushion any corns in these areas.
Removing Corns and Calluses. To remove a corn or callus, soak it in very warm water for 5 minutes or more to soften the hardened tissue, then gently sand it with a pumice stone. Several treatments may be necessary. Do not trim corns or calluses with a razor blade or other sharp tool. Unsterile cutting tools can cause infection, and it is easy to slip and cut too deep, causing excessive bleeding or injury to the toe or foot.
Medicated Solutions and Pads. There are numerous over-the-counter pads, plasters, and medications for removing corns and calluses. These treatments commonly contain salicylic acid, which may cause irritation, burns, or infections that are more serious than the corn or callus. Use caution with these medications. The following people should not use them:
- Patients with diabetes
- Patients with reduced feeling in the feet due to circulation problems or neurological damage
- Patients who do not have the flexibility or eyesight to use them properly
Bunions
A bunion is a deformity that usually occurs at the end of one of the five long bones (the metatarsal bones) that extend from the arch of the foot and connect to the toes. Most often bunions develop in the first metatarsal bone (the one that attaches to the big toe). A bunion may also develop in the bone that joins the little toe to the foot (the fifth metatarsal bone), in which case it is known as either a bunionette or a tailor's bunion.
A bunion typically develops in the following way:
- The big toe or the fifth ("pinky") toe is forced in toward the other toes, causing the head of the metatarsal bone to jut out and rub against the side of the shoe.
- The underlying tissue becomes inflamed, and a painful bump forms.
- As this bony growth develops, a bunion is formed as the big toe is forced to grow at an increasing angle toward the rest of the toes. One important bunion deformity, hallux valgus, causes the bone and joint of the big toe to shift and grow inward, so that the second toe crosses over it.
People born with abnormal bones in their feet are more likely to form a bunion. In addition, wearing narrow-toed, high-heeled shoes, which put enormous pressure on the front of the foot, may also lead to a bunion formation. The condition may become painful as extra bone and a fluid-filled sac grow at the base of the big toe.
Flat feet, gout, arthritis, and occupations (such as ballet) that place undue stress on the feet can also increase the risk for bunions.
Shoes and Protective Pads. Pressure and pain from bunions and bunionettes can be relieved by wearing appropriate shoes, such as the following:
- Soft, wide, low-heeled leather shoes that lace up
- Athletic shoes with soft toe boxes
- Open shoes or sandals with straps that don't touch the irritated area
A thick doughnut-shaped, moleskin pad can protect the protrusion. In some cases, an orthotic can help redistribute weight and take pressure off the bunion. Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections may offer some pain relief.
Surgery. If discomfort persists, surgery may be necessary, particularly for more serious conditions, such as hallux valgus. There are more than 100 surgical variations, ranging from removing the bump to realigning the toes.
The most common surgery, an office procedure known as bunionectomy, involves shaving down the bone of the big toe joint. In one procedure the surgeon uses a very small incision, through which the bone-shaving drill is inserted. The physician shaves off the bone, guided by feel or x-ray. This technique is not a cure, but patient satisfaction is high and results are long-lasting.
Click the icon to see an illustrated series detailing bunion removal.Click the icon to see an illustrated series detailing bunion removal.
More extensive surgeries may be required to realign the toe joint. Although there are variations of each, they generally involve one or more of the following:
- Osteotomy (cutting and realigning the joint). Long-term studies on osteotomies report that 90% of patients are satisfied with the procedure.
- Exostosectomy (removal of the large bony growth). This technique is only useful when there is no shift in the toe bone itself.
- Arthrodesis (removal of damaged portion of the joint, followed by implantation of screws, wires, or plates to hold the bones together until they heal). This is the gold standard procedure for very severe cases or when previous procedures have failed. Most patients report good results.
- Arthroplasty (removal of damaged portion of the joint with the goal of achieving a flexible scar). This technique offers symptom relief and faster rehabilitation than arthrodesis, but it can cause deformity and some foot weakness. Arthroplasty tends to be used in older patients. Biological or synthetic implants for supporting the toes are showing promise as part of this procedure.
- Tendon and Ligament Repair. If tendons and ligaments have become too loose, the surgeon may tighten them.
In severe cases, surgeons are testing bone grafts to restore bone length in patients who have had previous bunion surgeries or damage from osteoarthritis.
Complications, though uncommon in even the most complex procedures, can include:
- Continued pain
- Infection
- Possible numbness
- Irritation from implants used to support the bone
- An excessively shortened metatarsal bone
Recovery from more invasive procedures, such as arthrodesis or osteotomy, may take 6 - 8 weeks, and it can be that long before a patient can put full weight on the foot. In such cases, the patient will need to wear a cast or use crutches. Elderly patients may need wheelchairs.
Hammertoes
A hammertoe is a permanent deformity of the toe joint, in which the toe bends up slightly and then curls downward, resting on its tip. When forced into this position long enough, the tendons of the toe shrink, and the toe stiffens into a hammer- or claw-like shape.
Hammertoe is most common in the second toe, but it can develop in any or all of the three middle toes if they are pushed forward and do not have enough room to lie flat in the shoe. The risk is increased when the toes are already crowded by the pressure of a bunion. Conditions that increase the risk of hammertoe include:
- Diabetes
- Diseases that affect the nerves and muscles
Treatment for Hammertoe. At first, a hammertoe is flexible, and any pain it causes can usually be relieved by putting a toe pad, sold in drug stores, into the shoe. To help prevent and ease existing discomfort from hammertoes, shoes should have a deep, wide toe area. As the tendon becomes tighter and the toe stiffens, other treatments, including exercises, splints, and custom-made shoe inserts (orthotics) may help redistribute weight and ease the position of the toe.
Surgery. Patients with severe cases of hammertoe may need surgery. If the toe is still flexible, only a simple procedure that releases the tendon may be involved. Such procedures sometimes require only a single stitch and a Band-Aid. If the toe has become rigid, surgery on the bone is necessary, but it can still be performed in the doctor's office. A procedure called PIP arthroplasty involves releasing the ligaments at the joint and removing a small piece of toe bone, which restores the toe to its normal position. The toe is held in this position with a pin for about 3 weeks, and then the pin is removed. The procedure seems to have a high, lasting success rate.
Ingrown Toenails
Ingrown toenails can occur on any toe but are most common on the big toes. They usually develop when tight-fitting or narrow shoes put too much pressure on the toenail and force the nail to grow into the flesh of the toe. Incorrect toenail trimming can also contribute to the risk of developing an ingrown toenail. Other causes are:
- Injuries
- Abnormalities in the structure of the foot
- Repeated impact on the toenail from high-impact aerobic exercise
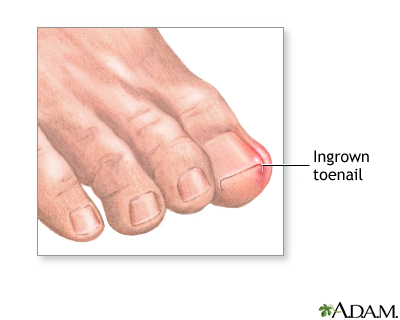
Caring for Toenails. Trim toenails straight across and keep them long enough so that the nail corner is not visible. If the nail is cut too short, it may grow inward. If the nail does grow inward, do not cut the nail corner at an angle. This only trains the nail to continue growing inward. When filing the nails, file straight across the nail in a single movement, lifting the file before the next stroke. Do not saw back and forth. A cuticle stick can be used to clean under the nail.
Treatments. To relieve pain from ingrown toenails, try wearing sandals or open-toed shoes. Soaking the toe for 5 minutes twice a day in a warm water solution of salt, Domeboro or Betadine can help. People who are at increased risk for infections, such as those with diabetes, should have professional treatment.
Antibiotic ointments may help treat ingrown toenails that are infected. Apply the ointment by working a wisp of cotton under the nail, especially the corners, to lift the nail up and drain the infection. The cotton will also help force the toenail to grow out correctly. Change the cotton daily, and use the antibiotic consistently.
In severe cases, more intensive treatments are needed. Surgery involves simply cutting away the sharp portion of ingrown nail, removing the nail bed, or removing a wedge of the affected tissue. Orthonyxia, a newer surgical technique that implants a small metal brace into the top of the nail, may be as effective as traditional surgical techniques for preventing ingrown toenails from recurring.
Nonsurgical methods can also treat ingrown toenails. One technique uses chemicals to remove the skin. Both sodium hydroxide and phenol may be used, but research shows that sodium hydroxide produces a better outcome and faster recovery than phenol. Other nonsurgical methods include using cauterization (heating), or lasers, to remove the skin.
Forefoot Pain
Forefoot pain refers to pain and discomfort felt toward the top of the foot. The rate of forefoot pain and deformity increases with age. When a cause cannot be determined, any pain on the ball of the foot is generally referred to as metatarsalgia.
Forefoot pain may be due to:
- Morton's neuroma
- Sesamoiditis
- Stress fractures
Morton's Neuroma
A neuroma usually means a benign tumor of a nerve. However, Morton's neuroma, also called interdigital neuroma, is not actually a tumor. It is a thickening of the tissue surrounding the nerves leading to the toes. Morton's neuroma usually develops when the bones in the third and fourth toes pinch together, compressing a nerve. It can also occur in other locations. The nerve becomes enlarged and inflamed. The inflammation causes a burning or tingling sensation and cramping in the front of the foot. Other causes of this condition include:
- Tight, poorly-fitting shoes
- Injury
- Arthritis
- Abnormal bone structure
Treatment for Neuromas. Pain from Morton's neuroma can be reduced by massaging the affected area. Roomier shoes (box-toed shoes), pads of various sorts, and cortisone injections in the painful area are also helpful. A combination of cortisone injections and shoe modifications provides better immediate relief than changes in footwear alone. Ultrasound-guided injection of alcohol might also provide relief from Morton's neuroma, research finds.
If these treatments are not effective, the enlarged area may need to be surgically removed. Success rates for this procedure seem to be high and provide long-term relief. Some numbness is common afterward, but it rarely bothers patients. Occasionally, the nerve tissue may re-grow and form another neuroma.
Sesamoiditis
Sesamoiditis is an inflammation of the tendons around the small, round bones that are embedded in the head of the first metatarsal bone, which leads to the big toe. Sesamoid bones bear much stress under ordinary circumstances; excessive stress can strain the surrounding tendons. Often there is no clear-cut cause, but sesamoid injuries are common among people who participate in jarring, high-impact activities, such as ballet, jogging, and aerobic exercise.
Treatment for Sesamoiditis. Rest and reducing stress on the ball of the foot are the first lines of treatment for sesamoiditis. A low-heeled shoe with a stiff sole and soft padding inside is all that is usually required. In severe cases, surgery may be necessary.
Stress Fracture
A stress fracture in the foot, also called fatigue or march fracture, usually results from a break or rupture in any of the five metatarsal bones (mostly the second or third). These fractures are caused by overuse during strenuous exercise, particularly jogging and high-impact aerobics. Women are at higher risk for stress fracture than men.
A fracture in the first metatarsal bone, which leads to the big toe, is uncommon because of the thickness of this bone. If it occurs, however, it is more serious than a fracture in any of the other metatarsal bones because it dramatically changes the pattern of normal walking and weight bearing.
Treatment for Stress Fractures. Patients should seek treatment if pain persists for 3 weeks. Treatment after that time may reduce the chances of returning to previous level of functioning. Surgery may be needed if conservative measures fail. In most cases, however, stress fractures heal by themselves if you avoid rigorous activities. Some health care providers recommend moderate exercise, particularly swimming and walking. It is best to wear low-heeled shoes with stiff soles. Occasionally, a health care provider may recommend wearing a walking "boot" (brace) to reduce pain and facilitate healing.
Heel Pain
The heel is the largest bone in the foot. Heel pain is the most common foot problem and affects 2 million Americans every year. It can occur in the front, back, or bottom of the heel. Types of heel pain include:
- Achilles tendinitis
- Bursitis of the heel
- Excess pronation
- Haglund's deformity
- Heel spur syndrome
- Plantar fasciitis
Each type of heal pain is described in more detail below. General treatment guidelines are as follows:
- The American Orthopaedic Foot and Ankle Society (AOFAS) suggests shoe inserts, medications, and stretching as a first line of therapy for heel pain. One study found that 95% of women who used an insert and did simple stretching exercises for the Achilles tendon and plantar fascia experienced improvement after 8 weeks.
- If these treatments fail, the patient may need prescription heel orthotics and extended physical therapy. Surgery may be an option if other methods have failed.
Achilles Tendinitis
Achilles tendinitis is an inflammation of the tendon that connects the calf muscles to the heel bone. It is caused by small tears in the tendon from overuse or injury. This condition is most common in people who engage in high-impact exercise, particularly jogging, racquetball, and tennis.
Of the people who engage in these activities, those at highest risk for this disorder are the ones with a shortened Achilles tendon. Such people tend to roll their feet too far inward when walking, and may bounce when they walk. A shortened tendon can be due to an inborn structural abnormality, or it can develop from regularly wearing high heels.
An inflamed or torn Achilles tendon causes intense pain and affects mobility.
Evidence is inconclusive about the best way to treat either acute or chronic Achilles tendinitis. Some approaches include:
Treatments to Relieve Pain and Reduce Inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen (Advil), may help ease pain and reduce inflammation. It is also helpful to apply ice for 20 - 30 minutes, four or five times a day. (Note: Corticosteroid injections are sometimes used, although evidence suggests they don't help very much, and they can pose a risk for rupture of the tendon.)
Gentle Stretching. Gentle calf muscle stretches may also help reduce pain and spasms. If the calf is swollen, elevate the leg. Exercise is safe when the heel is no longer swollen or tender, even if pain is still present. If pain increases with exercise, stop immediately.
Surgery vs. Nonsurgical Treatment. Chronic inflammation may lead to rupture of the Achilles tendon. If pain continues, the ruptured tendon will require a cast and perhaps surgery, called tendon transfer. Although some experts believe a cast without surgery is a sufficient treatment for such rupture, there is a chance the tendon may rupture again in the future, even after it heals. Some experts suggest surgery for active people and nonsurgical treatment for older people.
Surgery requires a long incision with a postoperative period of immobilization that can average 6 weeks. Complications can include a significant surgical scar, infection, and muscle atrophy, although surgery reduces pain and preserves foot function in the long term.
Bursitis of the Heel
Bursitis of the heel is an inflammation of the bursa, a small sack of fluid beneath the heel bone. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen (Advil), and steroid injections will help relieve pain from bursitis. Applying ice and massaging the heel are also beneficial. A heel cup or soft padding in the heel of the shoe reduces direct impact when walking.
Excessive Pronation
Pronation is the normal motion that allows the foot to adapt to uneven walking surfaces and to absorb shock. Excessive pronation occurs when the foot has a tendency to turn inward and stretch and pull the fascia. It can cause not only heel pain, but also hip, knee, and lower back problems.
Haglund's Deformity
Haglund's deformity, known medically as posterior calcaneal exostosis, is a bony growth surrounded by tender tissue on the back of the heel bone. It develops when the back of the shoe repeatedly rubs against the back of the heel, aggravating the tissue and the underlying bone. It is commonly called pump bump because it's often linked to wearing high heels. (It can also develop in runners, however.)
Treatment for Haglund's Deformity. Applying ice followed by moist heat will help ease discomfort from a pump bump. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen (Advil), will also reduce pain. Your doctor may recommend an orthotic device to control heel motion. Corticosteroid injections are not recommended because they can weaken the Achilles tendon.
In severe cases, surgery may be necessary to remove or reduce the bony growth. Studies show, however, that recovery from surgery is very long, and success rates vary. Experts advise patients to try all conservative measures before choosing surgery.
Plantar Fasciitis and Heel Spur Syndrome
Plantar fasciitis is a common foot problem that accounts for 1 million office visits per year. Plantar fasciitis occurs from small tears and inflammation in the wide band of tendons and ligaments that stretches from the heel to the ball of the foot. This band, much like the tensed string in a bow, forms the arch of the foot and helps serve as a shock absorber for the body.
The term plantar means the sole of the foot, and fascia refers to any fibrous connective tissue in the body. Most people with plantar fasciitis experience pain in the heel with their first steps in the morning. The pain also often spreads to the arch of the foot. The condition can be temporary, or it may become chronic if ignored. Resting can provide relief, but only temporarily.
Heel spurs are calcium deposits that can develop under the heel bone as a result of the inflammation that occurs with plantar fasciitis. Heel spurs and plantar fasciitis are sometimes blamed interchangeably for pain, but plantar fasciitis can occur without heel spurs, and spurs commonly develop without causing any symptoms at all.
Causes of Plantar Fasciitis. The cause of plantar fasciitis is often unknown. It is usually associated with overuse during high-impact exercise and sports. Plantar fasciitis accounts for up to 9% of all running injuries. Because the condition often occurs in only one foot, however, factors other than overuse are likely to be responsible in many cases. Other causes of this injury include poorly-fitting shoes, lack of calf flexibility, or an uneven stride that causes an abnormal and stressful impact on the foot.
Treatment Goals. The three major treatment goals for plantar fasciitis are:
- Reducing inflammation and pain
- Reducing pressure on the heel
- Restoring strength and flexibility
Embarking on an exercise program as soon as possible and using NSAIDs, splints, or heel pads, as needed, can help relieve the problem. Pain that does not subside with NSAIDs may require more intensive treatments, including leg supports and even surgery.
Exercises to Restore Strength and Flexibility. Stretching the plantar fascia is the mainstay therapy for restoring strength and flexibility. One exercise involves the following:
- Put the hands on a wall and lean against them.
- Place the uninjured foot on the floor in front of the injured foot.
- Raise the heel of the injured foot.
- Gently stretch the injured leg and foot.
With stretching treatments, the plantar fascia nearly always heals by itself but it may take as long as a year, with pain occurring intermittently. A moderate amount of low-impact exercise (such as walking, swimming, or cycling) also seems to be beneficial.
Treatment. Inflammation and pain is most commonly treated with ice and over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen. NSAIDs reduce pain and disability in people with plantar fasciitis when used with other techniques, such as night splints and stretching.
Corticosteroids are powerful anti-inflammatory agents. An injection of a steroid plus a local anesthetic (such as Xylocaine) may provide relief in severe cases of plantar fasciitis. (Steroid injections are not used for pain that is only due to heel spurs). For athletes or performers who need immediate relief, an effective method is to administer the steroid dexamethasone using a procedure called iontophoresis, which introduces the drug into the foot's tissue using an electrical current.
Several non-drug approaches can relieve pressure on the heel, including:
- Sturdy Shoes and Insoles. It is important to wear comfortable but sturdy shoes that have thick soles, rubber heels, and a sole insole to relieve pressure. (An insole with an arch support might also be helpful.) Cutting a round hole about the size of a quarter in the sole cushion under the painful area may help support the rest of the heel while relieving pressure on the painful spot. Heel cups are not very useful. When combined with exercises that stretch the arch and heel cord, over-the-counter insoles may offer the same relief as prescribed orthotics.
- Night Splints. Some evidence suggests that splints worn at night may be helpful for some people. One device, for example, uses an Ace bandage and an L-shaped fiberglass splint to keep the foot stretched while the patient is sleeping. This allows the muscle to heal. Although patient compliance may be better with custom-made prescribed orthotics than with tension night splints, it is believed that they are equally effective in improving pain. In addition, evidence suggests that nearly any splint, regardless of cost, is equally effective in about three-quarters of patients.
- Elevated Heels. Some people report relief from mild symptoms with the use of shoes or cowboy boots that have elevated heels. This approach, however, may not work in some people and is not recommended for anyone with a moderate-to-severe condition. (Heel cups have not been proven to be very useful.)
- Orthotics. For severe conditions, such as fallen arches or structural problems that cause imbalance, special insoles, called orthotics, may help. Custom orthotics are made to fit the patient's foot and individual clinical needs. (See "Insoles and Orthotics" section).
- Extracorporeal Shock Wave Therapy (ESWT). ESWT may be used as an alternative to surgery for patients who have not responded to other treatments. The therapy uses low-dose sound waves to injure the surrounding tissues in the heel, which is believed to trigger healing of the tissues that are causing the pain. Studies show that the treatment provides a very small reduction in heel pain without side effects. It can be considered as an option for patients who haven't responded well to extensive conservative treatment.
- Surgery. Surgery may be needed for some patients, typically those who have disabling heel pain that does not respond to other treatments for at least a year. A typical surgery is called instep plantar fasciotomy. It relieves pressure on the nerves that are causing pain by removing and therefore releasing part of the plantar fascia. A less invasive method uses a procedure called endoscopy, which requires smaller incisions. Wearing a below-the-knee walking cast after surgery for 2 weeks may reduce the need for pain relief and speed recovery time compared to the use of crutches.
- Botox. Studies show that injections of botulinum toxin (Botox), a protein used to temporarily paralyze certain muscles, reduce pain and improve patients' future ability to walk. More research is needed on this treatment.
Flat Feet
"Flat foot," or pes planus, is a defect of the foot that eliminates the arch. The condition is most often inherited. Arches, however, can also fall in adulthood, in which case the condition is sometimes referred to as posterior tibial tendon dysfunction (PTTD). This occurs most often in women over age 50, but it can occur in anyone. The following are risk factors for PTTD:
- Wearing high heels for long periods of time is a particular risk for flat feet. Over the years, the Achilles tendon in the back of the calf shortens and tightens, so the ankle does not bend properly. The tendons and ligaments running through the arch then try to compensate. Sometimes they break down, and the arch falls.
- Some studies have indicated that the earlier a person starts wearing shoes, particularly for long periods of the day, the higher the risk for flat feet later on.
- Other conditions that can lead to PTTD include obesity, diabetes, surgery, injury, rheumatoid arthritis, or the use of corticosteroids.
Some research suggests that flat feet in adults can, over time, actually exert abnormal pressure on the ankle joint that can cause damage. One indirect complication of flat arches may be urinary incontinence or leakage during exercise. The less flexible the arch, the more force reaches the pelvic floor, jarring the muscles that affect urinary continence. Nevertheless, whether flat feet pose any significant problems in adults is unknown.
Treatment for Flat Feet in Children. Doctors usually can't diagnose flat feet until a child is 6 years old. Children with flat feet typically don't have symptoms, and often outgrow the condition. Children who are experiencing symptoms might need to change shoes or wear arch supports. In rare cases, minimally invasive joint insert surgery may be an option.
Treatment for Flat Feet in Adults. In general, conservative treatment for flat feet acquired in adulthood (PTTD) involves pain relief and insoles or custom-made orthotics to support the foot and prevent progression.
In severe cases, surgery may be required to correct the foot posture, usually with procedures called osteotomies or arthrodesis that typically lengthen the Achilles tendon and adjust tendons in the foot. One procedure uses an implant to support the arch. These procedures have potential complications. Conservative methods should be tried first.
Abnormally High Arches
An overly-high arch ("hollow foot") can also cause problems. Army studies have found that recruits with the highest arches have the most lower-limb injuries and that flat-footed recruits have the least. Contrary to the general impression, the hollow foot is much more common than the flat foot.
Clawfoot, or pes cavus, is a deformity of the foot marked by very high arches and very long toes. Clawfoot is a hereditary condition, but it can also occur when muscles in the foot contract or become unbalanced due to nerve or muscle disorders.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome results from compression of a nerve that runs through a narrow passage behind the inner ankle bone down to the heel. It can cause pain anywhere along the bottom of the foot. It can occur with:
- Diabetes
- Back pain
- Arthritis
- Injury to the ankle
- Abnormal blood vessels
- Scar tissue that press against the nerve
Magnetic resonance imaging (MRI) and the dorsiflexion-eversion test can diagnose this syndrome.
Treatment for Tarsal Tunnel Syndrome. Specially designed shoe inserts called orthotics can relieve pain from tarsal tunnel syndrome because they help redistribute weight and take pressure off the nerve. Corticosteroid injections may also help. Surgery is sometimes performed, particularly if symptoms persist for more than a year, although its benefits are a matter of debate. Tarsal tunnel syndrome caused by known conditions, such as tumors or cysts, may respond better to surgery than tarsal tunnel syndrome of unknown cause. It can take months after this surgery for a person to recover and resume normal activities. Only experienced surgeons should perform tarsal tunnel syndrome surgery.
Foot Injury
If you suspect that you have broken or fractured bones in a toe or foot, call a doctor, who will probably order x-rays. Even if you can walk, you still might have a fracture. People are often able to walk even if a foot bone has been fractured, particularly if it is a chipped bone or a toe fracture.
Over-the-Counter Pain Relievers
Over-the-counter NSAIDs are commonly used to treat mild pain caused by muscle inflammation. Aspirin is the most common NSAID. Others include ibuprofen (Motrin, Advil, Nuprin, Rufen), ketoprofen (Actron, Orudis KT), naproxen (Aleve, Naprelan), and tolmetin (Tolectin). A gel containing ibuprofen can be applied to sore joints. Acetaminophen (Tylenol) is not an NSAID, and although it is a mild pain reliever, it will not reduce inflammation. It is important to note that high doses or long-term use of any NSAID can cause gastrointestinal disturbances with sometimes serious consequences, including dangerous bleeding. NSAIDs can also increase the risk of heart disease and stroke. This risk increases the longer you use them. No one should take NSAIDs for prolonged periods of time without consulting a doctor.
RICE (Rest, Ice, Compression, and Elevation)
The acronym RICE stands for rest, ice, compression, and elevation -- the four basic elements of immediate treatment for an injured foot.
- Rest. Patients should get off injured foot as soon as possible.
- Ice. This is particularly important to reduce swelling and promote recovery during the first 48 hours. Wrap a bag or towel containing ice around the injured area on a repetitive cycle of 20 minutes on, 40 minutes off.
- Compression. Lightly wrap an Ace bandage around the area.
- Elevation. Elevate the foot on several pillows.

Prevention
The American Podiatric Medical Association offers the following tips for preventing foot pain:
- Don't ignore foot pain -- it's not normal. If the pain persists, see a doctor who specializes in podiatry.
- Inspect feet regularly. Pay attention to changes in color and temperature. Look for thick or discolored nails (a sign of developing fungus), and check for cracks or cuts in the skin. Peeling or scaling on the soles of feet could indicate athlete's foot. Any growth on the foot is not considered normal.
- Wash feet regularly, especially between the toes, and dry them completely.
- Trim toenails straight across, but not too short. (Cutting nails in corners or on the sides increases the risk for ingrown toenails.)
- Make sure shoes fit properly. Purchase new shoes later in the day when feet tend to be at their largest, and replace worn out shoes as soon as possible.
- Select and wear the right shoe for specific activities (such as running shoes for running).
- Alternate shoes. Don't wear the same pair of shoes every day.
- Avoid walking barefoot, which increases the risk for injury and infection. At the beach or when wearing sandals, always use sunblock on your feet, as you would on the rest of your body.
- Be cautious when using home remedies for foot ailments. Self-treatment can often turn a minor problem into a major one.
- It is critical that people with diabetes see a podiatric physician at least once a year for a checkup. People with diabetes, poor circulation, or heart problems should not treat their own feet, including toenails, because they are more prone to infection.
Skin Creams and Foot Baths
Skin creams can help maintain skin softness and pliability. A pumice stone or loofah sponge can help get rid of dead skin.
Taking a warm footbath for 10 minutes two or three times a week will keep the feet relaxed and may help prevent mild foot pain caused by fatigue. Adding 1/2 cup of Epsom salts may increase circulation and add other benefits. Taking footbaths only when the feet are painful is not as helpful.
Proper Walking and Foot Exercises
In addition to wearing proper shoes and socks, walking often -- and properly -- can prevent foot injury and pain. The head should be erect, the back straight, and the arms relaxed and swinging freely at the side. Step out on the heel, move forward with the weight on the outside of the foot, and complete the step by pushing off the big toe.
Exercises specifically for the toe and feet are easy to perform and help strengthen them and keep them flexible. Helpful exercises include the following:
- Raise and curl the toes 10 times, holding each position for a count of five.
- Put a rubber band around both big toes and pull the feet away from each other. Count to five. Repeat 10 times.
- Pick up a towel with the toes. Repeat five times.
- Pump the foot up and down to stretch the calf and shin muscles. Perform for 2 or 3 minutes.
Preventing Foot Problems in Childhood
Early Development. The first year of life is important for foot development. Parents should cover their babies' feet loosely, allowing plenty of opportunity for kicking and exercise. Change the child's position frequently. Children generally start to walk at 10 - 18 months. They should not be forced to start walking early. Wearing just socks or going barefoot indoors helps the foot develop normally and strongly and allows the toes to grasp. Going barefoot outside, however, increases the risk for injury and other conditions, such as plantar warts.
Shoes. Children should wear shoes that are light and flexible, and since their feet tend to perspire, their shoes should be made of materials that breathe. Replace footwear every few months as the child's feet grow. Footwear should never be handed down. Protect children's feet if they participate in high-impact sports.
Shoes
In general, the best shoes are well cushioned and have a leather upper, stiff heel counter, and flexible area at the ball of the foot. The heel area should be strong and supportive, but not too stiff, and the front of the shoe should be flexible. New shoes should feel comfortable right away, without a breaking-in period.
Getting the Correct Fit
Well-fitted shoes with a firm sole and soft upper are the best way to prevent many problems with the feet. They should be purchased in the afternoon or after a long walk, when the feet have swelled. There should be 1/2 inch of space between the longest toe and the tip of the shoe (remember, the longest toe is not always the big toe), and the toes should be able to wiggle upward.
Stand when being measured, and have both feet sized, buying shoes that fit whichever foot is largest. Wear the same socks as you would regularly wear with the new shoes. Women who are accustomed to wearing pointed-toe shoes may prefer the feel of tight-fitting shoes, but with wear their tastes may adjust to shoes that are less confining and properly fitted.
The Sole
Ideally, the shoe should have a removable insole. Thin, hard soles may be the best choice for older people. Elderly people wearing shoes with thick inflexible soles may be unable to sense the position of their feet relative to the ground, significantly increasing the risk for falling.
The Heel
High heels are the major cause of foot problems in women. Although people believe that foot binding is a problem limited to Chinese women of the past, many fashionable high heels are designed to constrict the foot by up to an inch. Women who insist on wearing high-heeled shoes should at least look for shoes with wide toe room, reinforced heels that are relatively wide, and cushioned insoles. They should also keep the amount of time they spend wearing high heels to a minimum.
Laces
The way shoes are laced can be important for preventing specific problems. Laces should always be loosened before putting shoes on. People with narrow feet should buy shoes with eyelets farther away from the tongue than people with wider feet. This makes for a tighter fit for narrower feet and a looser fit for wider feet. If, after tying the shoe, less than an inch of tongue shows, the shoes are probably too wide. Adjust tightness both at the top and bottom of the shoe. If shoes with high arches cause pain, skip a few eyelets when lacing them. This should relieve pressure.
Breaking in and Wearing the Shoes
If shoes need breaking in, place moleskin pads next to areas on the skin where friction is likely to occur. Once a blister occurs, moleskin is not effective. Change shoes during the day, and rotate between different pairs of shoes. As soon as the heels show noticeable wear, replace the shoes or their heels.
Special-Purpose Footwear
Avoid extreme variations between exercise, street, and dress shoes.
Exercise and Sports. Shoes purchased for exercise should be specifically designed for a person's preferred sport. For instance, a running shoe should especially cushion the forefoot, while tennis shoes should emphasize ankle support. Athletic socks are almost as important as shoes. Experts often recommend padded acrylic socks.
Occupational Footwear. Because a number of occupations put the feet in danger, workers in high-risk jobs should be sure their footwear is protective. For example, non-electric workers at risk for falling, or whose work involves rolling objects or risk of shoe punctures, should wear shoes with steel toes and possibly other metal foot guards. Electric workers should wear footgear with no metal parts (or insulated steel toes) and rubber soles and heels. Chemical workers should wear shoes made of synthetics or rubber, not leather.
Shoes for Sports | |
Aerobic Dancing | Sufficient cushioning to absorb shock and pressure, which should be many times greater than shock from walking. Arches that maintain side-to-side stability. Thick upper leather support. Box toe. Orthotics may be required for people with ankles that over-turn inward or outward. Soles should allow for twisting and turning. |
Cycling | Rigid support across the arch to prevent collapse during pedaling. Heel lift. Cross-training or combo hiking/cycling shoes may be sufficient for the casual biker. Toe clips or specially designed shoe cleats for serious cyclers. In some cases, orthotics may be needed to control arch and heel and balance the forefoot. |
Running | Sufficient cushioning to absorb shock and pressure. Fully bendable at the ball of the foot. Enough traction on the sole to prevent slipping. Consider insole or orthotic with arch support for problem feet. |
Tennis | Allows side-to-side sliding. Low-traction sole. Snug fitting heel with cushioning. Padded toe box with adequate depth. Soft-support arch. |
Walking | Lightweight. Breathable upper material (leather or mesh). Wide enough to accommodate ball of the foot. Firm padded heel counter that does not bite into heel or touch anklebone. Low heel close to ground for stability. Good arch support. Front provides support and flexibility. |
Insoles
Insoles are flat cushioned inserts that are placed inside the shoe. They are designed to reduce shock, provide support for heels and arches, and absorb moisture and odor. In general, they can be very helpful for many people.
People respond very differently to specific insoles. What may work for one person may not work for another. Consider the thickness of socks when purchasing insoles to be sure they do not squeeze the toes up against the shoes. Insoles can be purchased in athletic and drug stores. Shoe stores that specialize in foot problems often sell customized, but more expensive, insoles. In general, over-the-counter insoles offer enough support for most people's foot problems. Most well-known brands of athletic shoes have built-in insoles.
Brands and Materials. There are many types of insoles available. They are composed of various materials, such as cork, leather, plastic foam, and rubber. Very effective insoles are now made from viscoelastic polymers (such as Sorbothane, Airplus, Spenco, Dr. Scholl's Massaging Gel, and others), which are gel-like materials that act both as liquids and solids.
Heel Cushions for Shortened Achilles Tendons. People who have developed short, tightened Achilles tendons (usually women who have worn high-heeled shoes for prolonged periods) should consider using heel cushions. Like insoles, heel cushions are inserted inside the shoes. They should be at least 1/8 inch thick, but not more than 1/4 inch thick.
Orthotics
For severe conditions, such as fallen arches or structural problems that cause imbalance, podiatrists or physicians may need to fit and prescribe orthotics, or orthoses, which are insoles produced to fit the patient's foot and match his or her clinical needs Orthotics are usually categorized as rigid, soft, or semi-rigid.
Before seeking prescription orthotics, people with less severe problems should consider testing the lower-priced, over-the-counter insoles.
Types of orthotics include:
- Rigid Orthotics. A rigid orthotics is used to control motion in two major foot joints that lie directly below the ankle. They are often used to prevent excessive pronation (the turning in of the foot) and are useful for people who are very overweight or have uneven leg lengths. Some experts warn that rigid orthotics may cause sesamoiditis or benign tumors from pinched nerves.
- Soft Orthotics. A soft orthotics is designed to absorb shock, improve balance, and remove pressure from painful areas. They are made from a lightweight material and are often beneficial for people with diabetes or arthritis. A soft orthotics needs to be replaced periodically, and because it is bulkier than rigid orthotics, it may require larger shoes.
- Semi-Rigid Orthotics. A semi-rigid orthotics is designed to provide balance, often for a specific sport. It is typically made of layers of leather and cork reinforced by silastic.
Resources
- www.apma.org -- American Podiatric Medical Association
- www.aofas.org -- American Orthopaedic Foot and Ankle Society
- www.acfas.org -- American College of Foot and Ankle Surgeons
- www.aapsm.org -- American Academy of Podiatric Sports Medicine
- www.apta.org -- American Physical Therapy Association
- www.diabetes.org -- American Diabetes Association
- www.arthritis.org -- Arthritis Foundation
- www.podiatrynetwork.com -- Podiatry Network
References
Baer GS, Keene JS. Tendon injuries of the foot and ankle. In: DeLee JC, Drez D Jr., Miller MD, eds. DeLee and Drez's Orthopaedic Sports Medicine. 3rd ed. Philadelphia, Pa: Saunders Elsevier;2009. Pp. 2171-2205:section D.
Bostanci S, Kocyigit P, Gurgey E. Comparison of phenol and sodium hydroxide chemical matricectomies for the treatment of ingrowing toenails. Dermatol Surg. 2007;33:680-685.
Del Toro, DR. Tibial Neuropathy (Tarsal Tunnel Syndrome). In: Frontera WR, Silver JK, eds. Essentials of Physical Medicine and Rehabilitation. 2nd ed. Philadelphia, Pa: Saunders Elsevier;2008. pp. 479-482.
Donley BG, Moore T, Sferra J, Gozdanovic J, Smith R. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int. 2007;28:20-23.
Frey C, Zamora J. The effects of obesity on orthopaedic foot and ankle pathology. Foot Ankle Int. 2007;28:996-999.
Gollwitzer H, Diehl P, von Korff A, Rahlfs VW, Gerdesmeyer L. Extracorporeal shock wave therapy for chronic painful heel syndrome: a prospective, double blind, randomized trial assessing the efficacy of a new electromagnetic shock wave device. J Foot Ankle Surg. 2007;46:348-357.
Hawke F, Burns J, Radford JA, du Toit V. Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst Rev. 2008;16:(3):CD006801
Heidelbaugh JJ, Lee H. Management of the ingrown toenail. Am Fam Physician. 2009;79(4):303-8.
Hughes RJ, Ali K, Jones H, Kendall S, Connell DA. Treatment of Morton's neuroma with alcohol injection under sonographic guidance: follow-up of 101 cases. Am J Roentgenol. 2007;188:1535-1539.
Kruijff S, van Det RJ, van der Meer GT, van den Berg IC, van der Palen J, Geelkerken RH. Partial matrix excision or orthonyxia for ingrowing toenails. J Am Coll Surg. 2008;206:148-153.
Lee SY, McKeon P, Hertel J. Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis. Phys Ther Sport. 2009;10:12-18.
Malay DS, Pressman MM, Assili A, Kline JT, York S, Buren B, Heyman ER, Borowsky P, LeMay C. Extracorporeal shockwave therapy versus placebo for the treatment of chronic proximal plantar fasciitis: results of a randomized, placebo-controlled, double-blinded, multicenter intervention trial. J Foot Ankle Surg. 2006;45:196-210.
The Ankle and Foot. In: Mercier, LR. Mercier: Practical Orthopedics, 6th ed. Philadelphia, Pa: Mosby;2008. pp.243-273.
Pasquina PF, Foster LS. Plantar fascitis. In: Frontera WR, Silver JK, eds. Essentials of Physical Medicine and Rehabilitation. 2nd ed. Philadelphia, Pa: Saunders Elsevier;2008. pp. 469-473.
Richardson EG. Disorders of the hallux. In: Canale ST, Beatty JH, eds. Campbell's Operative Orthopaedics. 11th ed. Philadelphia, Pa: Mosby Elsevier; 2007. pp. 4471-4575.
|
Review Date:
1/30/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |




